Did someone say milk and cookies? Or peanut butter and jelly, perhaps? We all know some matches are made in the heavens.
Speaking of ideal matches, when it comes to dentistry, dental bone grafts and dental implants come pretty close to the same analogy.
1. What is dental bone grafting and what are the benefits of the procedure?
Bone grafting, or dental bone grafting, is a minor surgical procedure to replace missing bone tissue in a particular area of the upper or lower jaw bone.
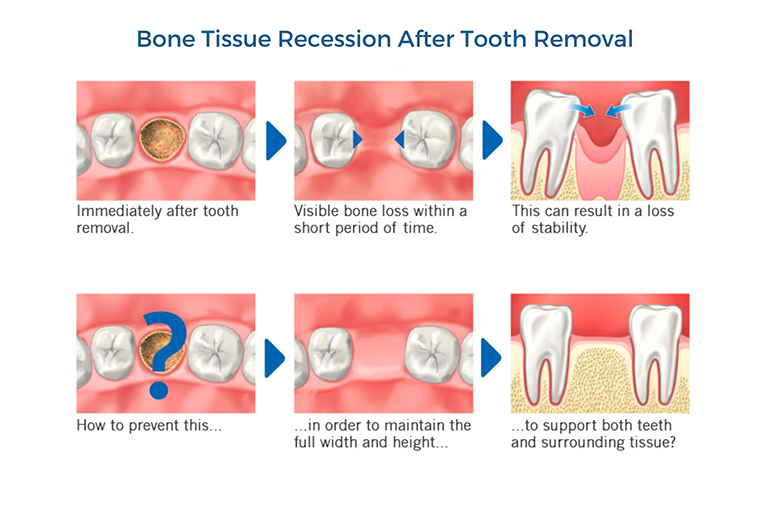
Bone tissue recession often occurs due to the lack of stimulation caused by the absence of the tooth root in the area after the removal of a tooth.
This target area or recipient site is usually the location where a dental implant is destined to be placed.
A key benefit of this procedure is that it utilizes the human body’s incredible ability to regenerate or regrow certain areas if provided with the right environment and conditions.
Dental bone grafts do just that.
They provide the near-ideal conditions (and space) for natural bone cells to get to work and grow in the target location and gradually replace the bone graft material – forming a dense area of new bone that is unified with the surrounding jaw bone tissue.
2. What is the procedure for dental bone grafting?
The procedure for bone grafting, although theoretically a simple one, requires a fair bit of skill on the part of your dental implantologist (someone who has specialized in all things dental implants).
The entire procedure can be summed up in the following steps:
1 – Dental and Medical History
An accurate history of your previous dental office visits, treatments (crowns, fillings, root canals, etc.), diagnoses, and procedures are updated and maintained in the dental office records for future reference and when planning new treatments.
These details can impact future treatment directions of your new treatment plan and goals.
For instance, a history of past radiation therapy may be relevant for determining the health of surrounding bone to avoid chances of graft failure.
If you happen to go to a new dentist, she or he would also require a medical history, including any medications you are taking.
As many medications can interact with certain types of anesthesia (used to numb your teeth, gums, and jaw) or with medicines that the dentist may prescribe after treatment.
2 – Oral Exam Stage
Your dentist performs a general oral checkup to assess the health of your gums, teeth, and jaw.
At this stage, the dentist may order some CT scans or dental x-rays to evaluate the extent of bone loss in the target area.
3 – Personalized Treatment Plan
After assessing your oral health status and discussing all appropriate treatment options, the dentist will draft a treatment plan.
The personalized treatment plan best meets your oral health objectives and requirements.
4 – Surgical Steps
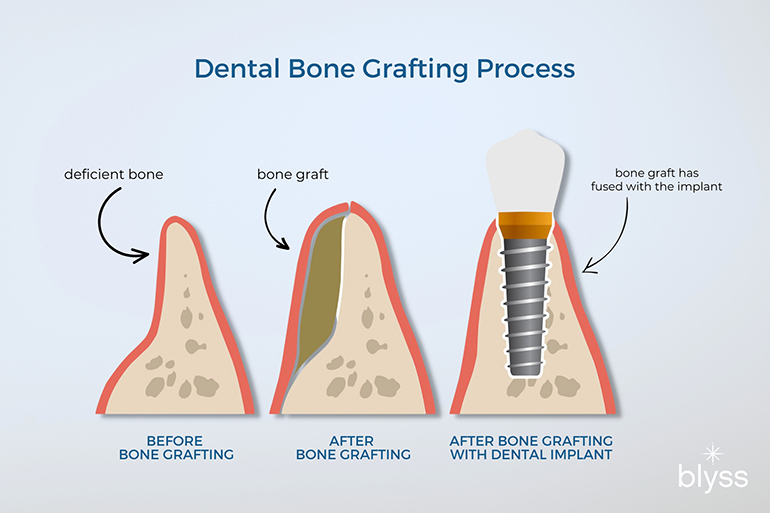
Dental bone grafting can provide greater stability and support for dental implants, bridges, and dentures, as well as help prevent further bone loss.
- Step 1: The dentist numbs the target area (tooth removal and future dental bone graft site) with local anesthesia.
- Step 2: Then, she or he will make a small surgical incision in your gums to expose the tooth and surrounding bone.
- Step 3: The dentist may then use special (tooth shape specific) forceps to first grip the crown to loosen and pry the (target) tooth (to be removed) from its socket. Alternatively, special surgical instruments may be used (that rely on the lever and fulcrum mechanics) to achieve the same effect as the toothed forceps.
- Step 4: Once the tooth extraction procedure is complete, a small portion of gum tissue is pulled back to make the underlying jawbone visible.
- Step 5: After sufficiently cleaning the area, your dentist will finally add the bone grafting material to the recipient site in the jaw bone. In some cases, the dentist may opt for covering the area with another synthetic layer on top of the bone graft to secure it in place. The gums are then drawn back over the bone graft area
- Step 6: Last but not least, the incision is then resolved with stitches to hold both ends of the tissue in place.
3. Is bone grafting painful?
While the grafting procedure does not usually entail a painful experience, expect some discomfort a few hours after the procedure once the effect of anesthesia wears off.
However, your dentist will usually prescribe an over-the-counter pain relief medicine to counter that.
The pain relievers will minimize any residual discomfort or pain during the three to four days following the procedure.
4. What are the risks associated with it OR What can go wrong with bone grafting?
After going through a bone grafting procedure, you may experience mild to moderate pain, bruising, and swelling.
Unless the graft is infected or fails due to some other health-related issues or post-surgery care, the good news is that all other events can be effectively managed with pain relief medicines.
In some instances, your dentist may also prescribe antibiotics just to be sure.
5. When do you need bone grafting? For what procedures?
Anyone faced with the problem of addressing the loss of a significant volume of bone in their jaw (in one or more areas) is usually recommended a bone grafting procedure.
This is especially true if you and your dentist have planned advanced dental rehabilitative and/or restorative treatments inside your mouth.
These may include the following common clinical situations:
Removing a Tooth from the Jaw
Placing a bone graft during the tooth extraction healing stages, immediately after the tooth has been removed from the jaw bone, helps preserve the bony architecture of the socket.
Opting for a Dental Implant to Replace a Missing Tooth
If there was no tooth (for some time) at a planned location in the jaw that is to anchor and support a dental implant, there is a high probability that the jaw bone is not as dense and voluminous as it used to be.
In this instance, bone grafting can help restore some of that lost jaw bone volume.
Which will, in turn, provide a stable bony platform to support the healing stages of a dental implant-based prosthesis.
Going for Dentures
Here you can picture the same scenario as above.
Only this time, the goal is to achieve the same amount of bone volume enrichment and expansion spread out over a larger area of the jaw bone.
One that will support the entire length and width of a denture.
Addressing Moderate to Advanced-Stage Gum or Periodontal Disease
A long-standing infection of the gums or gum disease can wreak havoc on the bone surrounding the teeth.
This can eventually lead to the loss of supporting bone around the teeth. And the teeth become loose in their sockets.
Expertly placed bone grafts around the affected teeth promote bone healing and reduce overall tooth mobility.

Dental bone grafting is necessary to restore the jawbone structure damaged by periodontal disease, trauma, or congenital defects.
6. Do all extractions need bone grafting? Is bone grafting necessary?
Let’s say the jury is still out on this one. Bone grafting is often necessary if you are getting a dental implant after your extraction.
Generally speaking, whenever there is a tooth extraction event or its voluntary removal from the tooth socket (the leftover hole in the jaw bone after the tooth has been removed), there is an accompanying rapid loss of bone in and around that area.
In this instance, resorting to dental bone graft materials for preserving the tooth socket region after the loss of a tooth is done on a case-to-case basis.
Given specific clinical cues, your dentist may order dental x-rays to assess the level of bone loss in the tooth socket area.
If there is evidence of a particular kind of bone loss at the tooth extraction site, such as a vertical bone loss event (VBE) in advanced-stage gum disease, then the dentist may use a bone graft to preserve bone volume and health to prevent further loss of tissue.

Left untreated, vertical bone loss event (VBE) can cause significant damage to supporting structures such as teeth, gums, and jaw bones.
More importantly, it’s important to remember that no ultimate bone graft material has a clear edge over others in terms of superior (and predictable) bone and gum line preservation after tooth loss.
7. Does a bone graft reduce the chances of a dry socket after tooth extraction?
After removing a tooth from its bony socket, there may be a chance to develop a condition referred to as a dry socket.
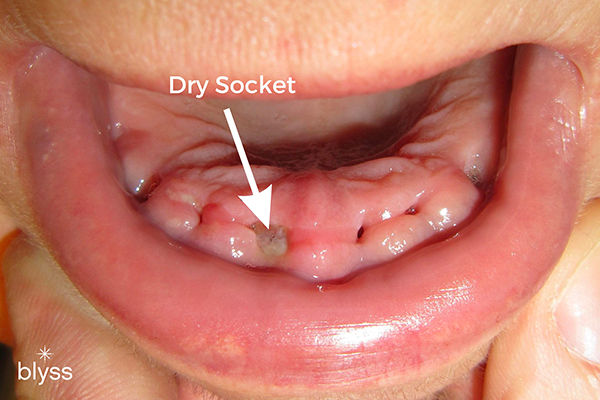
Prevent dry socket by avoiding activities that dislodge clots, such as smoking or consuming carbonated drinks following an extraction procedure. If left untreated, dry sockets can lead to more serious problems, such as infection or delayed healing of the tooth extraction site.
Generally, the chances of a dry socket scenario happening are less than 5% of everyday tooth extractions.
However, the percentage increases exponentially if lower jaw bone extractions in general and wisdom teeth, in particular (more than 35%).
If a dry socket does manifest after a tooth extraction, then the resulting scenario is usually a painful one.
However, it’s pertinent to note that not every painful socket leads to a dry socket scenario.
Having a few days of pain and discomfort after your tooth extraction is completely normal.
Dentists employ various techniques to close extraction wounds in certain groups of patients – who may be more susceptible to developing a dry socket.
They may include using dissolvable stitches and placing spongy collagen protein plugs and bone grafts.
Strictly speaking, dry sockets can still happen after receiving a bone graft. However, the likelihood of this is significantly lower.
8. What are the different types of bone grafting materials? Where do they come from? In what situations are they used?
For the sake of simplicity and clarity, let’s group the major types of bone grafts and substitute materials in dentistry in the categories below:
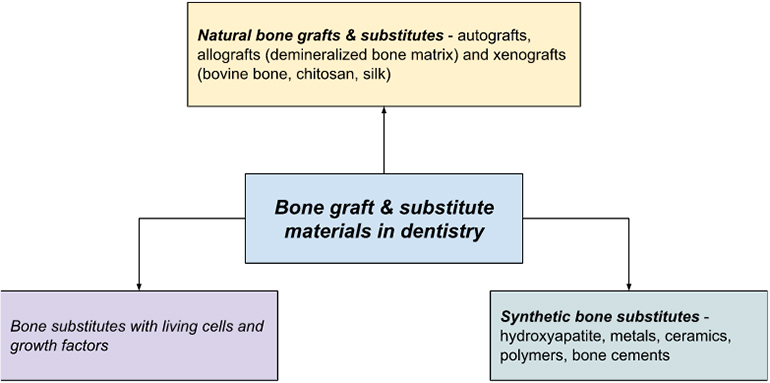
Autografts
The term autograft means that the bone graft is from the patient’s own body. This may involve a secondary surgical procedure for removing bone from another site in the patient’s body (such as the back part of the upper or lower jaw bone).
Allografts
These are bone grafts from other living donors or cadaveric bone sources.
Xenografts
These are bone grafts from species other than humans (such as cows, sheep, etc.).
Synthetic Bone Grafts
They usually occur as specially designed cement, bone material like crystals, and rubber-textured polymers.
As you have probably noticed, there are quite a few options out there when it comes to different types of dental bone graft materials.
But don’t get overwhelmed just yet. Each type of bone graft has its own set of pros and cons.
Up to 90% of all bone grafting procedures globally use a natural bone graft or a substitute material.
There is definitely a preference for using freeze-dried allografts in most dental bone grafting procedures.
As it allows for the many problems with autografts, such as a second surgical procedure to get bone, to be done away with.
Usually, a combination of allografts and xenografts (derived from other living things – animal, insect, or plant sources) are most commonly used for stimulating bone formation prior to installing a dental implant and for addressing bone defects in advanced-stage gum disease.
This is because allografts are safe, i.e., they induce little to no immune reaction in most cases.
More importantly, they are available in various forms, such as complete bone segments, chips, wedges, and powder, to name a few.
The versatility of allografts makes them suitable for numerous medical applications involving bone deficiencies in the mouth.
Be that as it may, your dentist will carefully discuss all available options and alternatives with you.
9. Is the use of cadaver bone common? What about safety and ethical concerns?
Allografts often include the use of cadaver bones as a source for bone grafts.
Allografts can be a combination of bone from cadaveric sources and compatible living donors.
Regarding ethical concerns about using cadaver-sourced bone grafts, professional regulatory bodies such as the American Dental Association have established ethical guidelines in place for all dental care providers.
This falls in line with one of the crucial tenets of dental and medical practice that acknowledges the patient’s (your) ability to play an active role in determining their treatment options in accordance with their individual views, desires, beliefs, and choices.
All treatment options in dentistry, including bone grafts, are considered carefully with respect to their constitution and source before being advised and delivered to patients as part of the final treatment plan.
Some patients voice safety-related concerns regarding the transmission of infection when using allograft bone graft materials.
But these are mostly far removed since efficient cleaning and sterilization techniques have come to the fore.
Be that as it may, you and your dentist can make a collective decision regarding a suited bone graft material you are comfortable receiving.
One that is aligned and acceptable to you in accordance with your cultural, religious, or spiritual beliefs.
10. What is the recovery process like after a dental bone grafting surgery? How long is the healing time?
After a dental bone graft is in place, expect some pain and swelling. This is completely normal.
Most symptoms usually go away in a week or two. However, it can take anywhere between 4 to 6 months to tick the completely healed checkbox.
This variable time scale is assigned after taking several factors into consideration (which vary for everyone since we’re all unique!)
These include:
- the location of the grafting site
- the size of the bone defect
- the overall health status of the patient
- your body’s unique healing capabilities
11. What happens if my bone grafting procedure fails?
The success rate for a fully integrated dental bone graft is quite high.
Yet, as with any dental/medical procedure, there is always an off chance that things don’t turn out quite as planned.
Here are some signs to watch out for to know if your dental bone graft is taking a turn for the worst:
- Pain or swelling at the graft site that does not improve or increase in intensity after the first 5 to 7 days.
- Gums pulling away from the bone graft area
- No appreciable positive change in the jaw bone in terms of bone gain.
In any or all of the above scenarios, you should give your dental clinic a call to schedule a visit.
12. How much does dental bone grafting cost on average, and how can patients save money on this procedure?
Considering the combined treatment costs that one may incur if gum disease is allowed to progress unchecked (with accompanying loss of bone mass and volume), a bone graft can be relatively inexpensive in comparison.
A standard (allogenic or synthetic bone-based) bone graft can fall in the ballpark of $250 to $1200.
The reason for this wide variation in price points is the different requirements of every case in terms of:
- The type of bone graft used
- Amount of the bone graft material used (depending on the size of the bone defect)
- Level of difficulty of access to the bone graft site
- The number of sites planned to receive a bone graft
- Skill/specialization level of the dental professional attempting the bone graft procedure (general dentist or a periodontist, for instance)
- Level of anesthesia administered (local or general)
But there is good news on the horizon.
Check out some of our insider super-saver tips if you are looking to shave off some dollars from your bone graft invoice (who isn’t right? We get it).
For starters, look into the details of your dental insurance, which may cover a significant chunk of the procedure.
Look around for dental practices outside your immediate neighborhood for better deals.
As a general rule, a specialist such as an oral surgeon is typically more expensive than a general dentist when it comes to advanced dental procedures such as placing bone grafts.
13. Are there any alternatives to dental bone grafting that achieve similar results for patients in need of surgery to improve their oral health?
Without adequate levels of bone volume at the target site, it’s not possible to place a standalone dental implant (or any other long-lasting dental prosthesis, for that matter).
Every dental implant requires good and healthy (surrounding) gum and bone tissue support to deliver its best years of service.
There is no best alternative to bone grafting procedures. It’s more about how best the dentist can resolve a bone volume issue in light of a patient’s dental history.
Here are some alternatives to bone grafting that dentists recommend after careful evaluation of your case:
Full-arch or Full-mouth Prosthesis
This method of restoring the dental arch relies on multiple dental implants strategically placed in the jaw bone in areas with sufficient bone.
The balanced placement of these implants in the dental arch allows them to work together (in synergy) to support a full-arch dental prosthesis without resorting to bone grafts.

Full-arch or full-mouth prostheses are designed to fit perfectly into each patient’s mouth and provide a natural-looking appearance along with improved chewing capabilities compared to traditional dentures or bridges.
Zygomatic or Cheekbone Implants
As the name implies, this type of prosthesis attaches to the cheekbones on either side using 2 metal connections that support full-arch dental prostheses in the upper jaw.
Zygomatic implants are usually for patients experiencing severe gum and bone loss due to large bone defects and/or advanced-stage generalized gum disease.
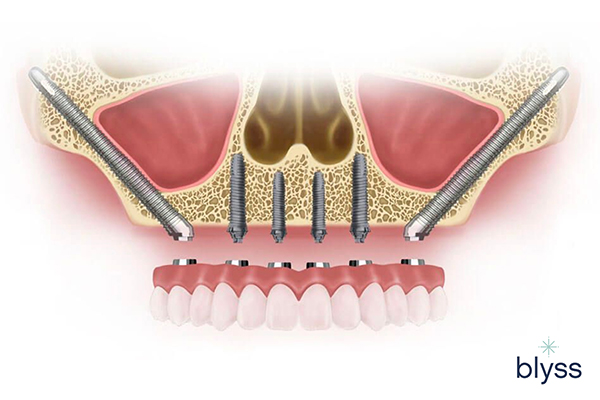
Zygomatic implants typically consist of a titanium post inserted into the jawbone, with a connecting abutment attached to secure a dental prosthetic.
All-on-4 Dental Implants
A modification of the full mouth prosthesis approach, this alternative-to-bone graft treatment uses the strategic and specific placement of 4 dental implants on the front jaw for supporting a fixed dental bridge
In all such cases, the long-term chances of success may be higher than resorting to bone grafting.
As these techniques make use of sound and existing natural bone in the mouth and cheekbones.
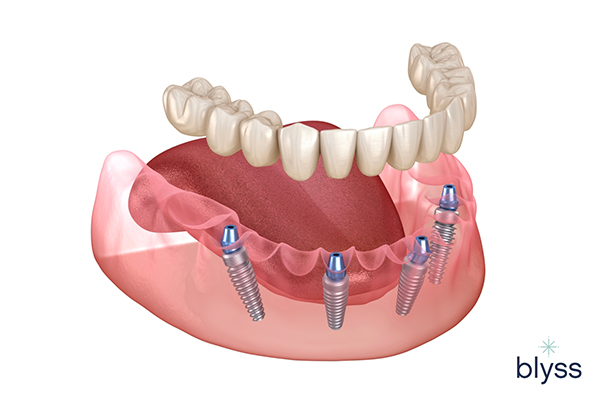
Due to their high success rate, All-on-4 implants have become popular for those seeking a secure replacement for missing teeth.
Conclusion – Final Notes
Still a little confused about opting for a dental bone graft procedure? We understand you may still have more questions.
Well, we have answers!
Learn more about bone grafting with Team Blyss.
Visit us at www.blyssdental.com or give us a call at 858-799-0570 to book your free consultation today.
References
- Zhao R, Yang R, Cooper PR, Khurshid Z, Shavandi A, Ratnayake J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules. 2021; 26(10):3007. https:
//doi.org/ 10.3390/ molecules 26103007 - Stumbras, A., Kuliesius, P., Januzis, G., & Juodzbalys, G. (2019). Alveolar Ridge Preservation after Tooth Extraction Using Different Bone Graft Materials and Autologous Platelet Concentrates: a Systematic Review. Journal of Oral & Maxillofacial Research, 10(1). https://doi.org/
10.5037/ jomr. 2019.10102 - Bone Augmentation and Tips for a Quick Recovery: El Paso Periodontics & Implant Specialists: Periodontists. (n.d.). https://
www.epimplant.com/ blog/bone-augmentation -and-tips-for-a- quick-recovery - Lau, B. Y., Johnston, B. D., Fritz, P. C., & Ward, W. E. (2013). Dietary Strategies to Optimize Wound Healing after Periodontal and Dental Implant Surgery: An Evidence-Based Review. The Open Dentistry Journal, 7, 36-46. https://
doi.org/10.2174/ 1874210601307010036 - Bone Grafting. (2020, January 3). Johns Hopkins Medicine. https://
www.hopkinsmedicine.org/ health/treatment-tests-and -therapies/ bone-grafting - Rose LF, Rosenberg E. Bone grafts and growth and differentiation factors for regenerative therapy: a review. Practical Procedures & Aesthetic Dentistry : PPAD. 2001 Nov-Dec;13(9):725-34; quiz 736, 721-2. PMID: 11862923
- Balaji, V. R. (2020, July 1). Bone grafts in periodontics Balaji V R, Manikandan D, Ramsundar A – Matrix Sci Med. https://
www.matrixscimed.org/ article.asp?issn=2521-0807; year=2020;volume=4; issue=3;spage=57;epage=63; aulast=Balaji - (2008). Use of Allogeneic Bone Graft in Maxillary Reconstruction for Installation of Dental Implants. Journal of Oral and Maxillofacial Surgery, 66(11), 2335-2338. https://
doi.org/10.1016/ j.joms.2008.06.006



